#HealthyPeachy Perlmutter Cancer Center Medical Oncologist Advances Innovative Clinical Trials for Breast Cancer
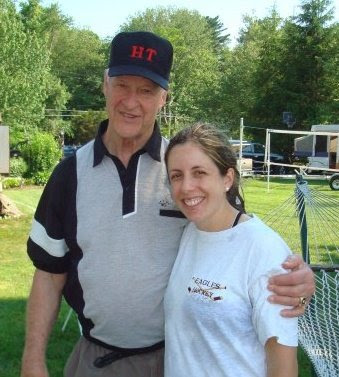
Nancy Chan, MD, a medical oncologist who treats people with breast cancer, joined NYU Langone Health's Perlmutter Cancer Center in September 2021 after spending seven years at Rutgers Cancer Institute as the co-leader of breast oncology. Dr. Chan is currently seeing patients at Perlmutter Cancer Center—34th Street and is part of the Breast Cancer Center. As director of breast cancer clinical research at Perlmutter Cancer Center, she brings the clinical knowledge learned from patients to colleagues who are developing new methods to understand and manage breast cancer.
Nancy Chan, MD
Dr. Chan discusses her new role at Perlmutter Cancer Center, clinical trials she is conducting, and more.
Can you tell us about your role as director of breast cancer clinical research?
One of the most important aspects of my role as director of breast cancer clinical research is to ensure that we have a constant, dynamic flow of clinical trials that are applicable to our very diverse patient population. These include trials in the early and metastatic settings, as well as in the maintenance setting for women who are cancer survivors, since there are clinical trials aimed at improving their quality of life. These trials encompass everything that you could think of that a person with breast cancer deals with, including side-effect management.
On a daily basis we are approached by either pharmaceutical companies or cooperative groups for clinical trial opportunities. There are many different trials that we can open, and my job is to select and curate the clinical trials that best serve our patient population and that allow patients to go on trials more easily.
There have been several studies done to look at why, across the nation and particularly at major cancer centers, less than 10 percent of patients ever go on a clinical trial. My job is also to dispel some of the stigma that surrounds being enrolled in a clinical trial. For example, people might think a clinical trial is the end of the road for them or that they are being used as a guinea pig. Also, being assigned to a placebo arm of a trial can be scary. We spend a lot of time in our clinic talking with patients to dispel some of those things.
How are you choosing clinical trials that meet the diverse patient populations that Perlmutter Cancer Center serves?
NYC Health + Hospitals/Bellevue is probably as diverse as you can get, and the patient population there is very different than at other sites in the NYU Langone Health and affiliated network. We see a lot of different and very interesting pathologies at Bellevue, which in many cases has to do a lot with access to care. We see patients coming in with later-stage cancers. We want to make sure that our clinical trials portfolio also covers those patients.
People come from all over the world to seek care at Bellevue and Perlmutter Cancer Center. I've done a lot of telemedicine visits with patients as far away as Europe and the Caribbean who are looking to New York City and Perlmutter Cancer Center as a hub for advanced cancer care. Each of these patients is diverse in different ways, and our clinical trials have to encompass all of the populations that we serve.
You have a special interest in phase 1 clinical trials. What is their importance for treating people with breast cancer?
The other hat that I wear is as a member of the novel therapeutics team at Perlmutter Cancer Center.
We generally are able to provide our patients with breast cancer a good quality of life, and for many years in many different cases. Each type of breast cancer is different, and in the metastatic setting, we have patients who have been through multiple lines of prior therapy.
For those patients, our goal obviously is to find them effective therapy. They always need to be on some therapy because they have metastatic disease, but often the breast cancer–specific trials may exclude them because they've had more than four or five lines of therapy, which is the cutoff for eligibility in many trials. So, what do we have to offer for our patients who are still in really good shape, have a good quality of life, and who are on their ninth line of therapy? It is those patients for whom we turn to our phase 1 studies.
When I screen a patient for a breast cancer trial, even if they haven't had eight or nine lines of therapy, I keep the phase 1 trials in mind because there may be a specific tumor mutation that a patient has that, if we can match that mutation to a specific targeted drug, then even if it's not a breast cancer–specific clinical trial, the patient may respond because we're treating according to their underlying genomic biology. That offers patients another avenue for early access to potentially effective drugs.
In Long Island and in Brooklyn, we're expanding our breast cancer research program. NYU Langone Hospital—Long Island and NYU Langone Hospital—Brooklyn are very robust sites. And we now have phase 1 clinical trials that cover not just people with breast cancer, but also other tumor subtypes. These other clinical trials are very important because they provide access to patients who otherwise would probably have to travel to Manhattan to get access to these studies.
What are some of the clinical trials that you have been conducting?
I have been very fortunate to participate and be one of the co-investigators on an upcoming trial coordinated by the Cancer Therapy Evaluation Program (CTEP), which is the early drug development branch of the National Cancer Institute (NCI). This is a very interesting study that combines radium-223 with a standard of care chemotherapy agent, paclitaxel, which is commonly utilized for treatment of breast cancer. Radium-223 is an isotope of radium that emits alpha particles specific for people with cancer that has metastasized to the bone. Essentially, this is a clinical trial combining a bone-targeting agent with systemic chemotherapy to potentiate the anti-tumor effects. Paclitaxel also targets breast cancer outside of the bone. Therefore, for people who have multiple sites of disease throughout the body, this may be a useful combination. This study is open and currently accruing at multiple NCI-designated cancer centers across the nation.
We have another study, part of the Big Ten Cancer Research Consortium, that is studying pembrolizumab combined with fulvestrant to treat hormone-positive breast cancer. Immunotherapy, which is more widely used in triple-negative breast cancer, is not commonly studied in hormone-positive breast cancer. The majority of our patients have hormone-positive breast cancer, both in the early and metastatic settings, and that's an area of interest that I want to explore to understand which patients will respond to immunotherapy. I presented that investigator-initiated trial in a poster session at the 2021 San Antonio Breast Cancer Symposium.
I presented another investigator-initiated trial in a poster session at that meeting on a study that recently completed accrual, which concluded that four cycles of neoadjuvant liposomal doxorubicin and carboplatin were found to be just as effective, but less toxic, than standard chemotherapy regimens.
What should people expect when they come for care at Perlmutter Cancer Center?
When I think about the different hats that I wear in the job that I do, the patient care part of it is so important. I love to get to know patients and not just their breast cancer history and how they were diagnosed. I take very good notes on how they were diagnosed, but also who they are and what they do. I ask them about their families and what's important to them. What are the relevant things that are going on in their lives? I have found that when you give time to patients and dive deeper into who they are, they really open up to you.
For example, I just met a young patient who started to tell me the story about her breast cancer diagnosis and told me something about her family history that she hadn't revealed to anyone else. A close family member had died a year earlier from breast cancer and that caused a lot of trauma. The diagnosis of breast cancer in a patient is traumatic enough, but to have also experienced it with an immediate family member is devastating. And this patient carried that burden with her through her own cancer diagnosis. That is just one example of really getting to know people.
With my patients, we come up with a treatment plan together, taking all the information we have from the breast cancer—from the pathology and from their history—and incorporating that into the person they are. That is something that I love to do and is truly important because that's what makes people feel that you truly care. At Perlmutter Cancer Center, across the board, this is what I see from my colleagues. The way that we approach a person with breast cancer is not just the breast cancer, but the person as a whole.